
As Russia exits the first wave of its coronavirus epidemic, officials risk new outbreaks by basing decisions on bad data
Мы рассказываем честно не только про войну. Скачайте приложение.
Based on multiple mathematical models, Russia’s coronavirus outbreak peaked on May 18 (several days after the epidemic peaked in Moscow). In this context, “peaking” signifies that the number of new cases has fallen below the number of patients recovering or dying from COVID-19. In other words, pressure on the medical system is gradually easing. This welcome news makes it tempting to begin lifting painful containment measures, but in most regions across Russia that likely remains premature. At the same time, unfortunately, the quality of the statistical data needed to make decisions about weakening quarantine restrictions has deteriorated in recent weeks, due to the flawed methodology proposed by federal regulators for calculating the epidemic’s most important indicators. As a result, many regions of Russia risk unleashing a second wave of coronavirus.
What’s an epidemiological peak and how do we know Russia has reached it?
A peak is the turning point in an epidemic when the number of people recovering or dying from a disease becomes greater than the number of new infections. Reaching the turning point means pressure on the healthcare system — particularly ICUs — has started to recede.
In late April, Meduza reported on forecasts using data-driven models for predicting the course of the COVID-19 epidemic, relying specifically on official state data (which was virtually useless at the start of the outbreak in the absence of other quality indicators and before enough information accumulated). Based on that earlier model, Moscow’s coronavirus outbreak would have peaked in mid-May, while the epidemic nationwide would have peaked around May 20.
The model uses only data on officially registered coronavirus infections, exploring the dynamics of the natural logarithm of the ratio of recently infected patients and fatalities. The number of recovered patients (plus deaths) can be represented as the number of registered cases with a shift of 12–15 days ahead (the average duration of a coronavirus infection, when the vast majority of patients recover, though some die). The American and Chinese scholars who pioneered this model say the “slope” of this relationship records all the epidemic’s parameters that appear to be hidden in official data: restrictive measures, changes in testing efficiency, and the epidemic’s reproduction rate at different times.
The points on the graph below are the natural logarithm of the ratio of registered cases and the number of recovered or killed patients (in other words, the number of cases 15 days earlier) for each day, placed on straight lines (with deviations) to represent the best linear approximation. When enough data has been accumulated (you need at least several weeks), the line can be extended into the future. When the line passes through “zero,” the epidemic has peaked. The model’s authors say this methodology has demonstrated predictive power in China, South Korea, and several European countries.
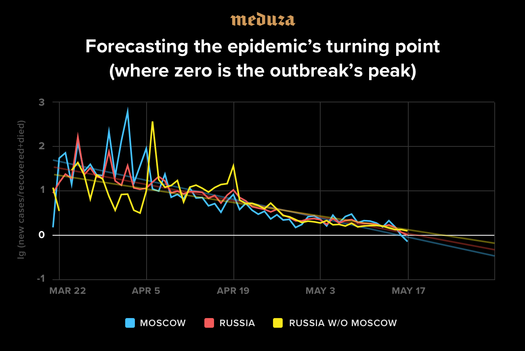
In Russia, the model’s prediction was also accurate. As demonstrated in the graph above, the first wave of Moscow’s coronavirus outbreak peaked on Sunday, May 17. Nationally, Russia’s epidemic peaked a day later, and regions outside the capital should reach their turning point before the end of the week. It is important to note, however, that the model does not accurately predict new infections in recent days, when regional officials across Russia began easing containment restrictions. The model cannot be used to predict the start of a second wave of coronavirus cases. The number of active infections in Russia apparently started falling in early May, as demonstrated by this graph, though the shift was not immediately visible.
Other studies based on different principles also confirm these models. Research by scholars at the Los Alamos National Laboratory and the University of Melbourne also predicted that Russia’s coronavirus epidemic would peak on May 18.
Admittedly, medical experts have identified more and more “strange data” coming from regional health officials about new cases, but these aberrations are limited by the fact that two-thirds of Russia’s officially recorded COVID-19 cases have been in Moscow, the Moscow region, St. Petersburg, and the Nizhny Novgorod region, where the statistics remain generally plausible.
What now? Is it time to lift containment measures?
The authorities have to be especially careful. Now comes the most difficult stage: easing restrictions while avoiding an immediate second wave of infections. Researchers at the University of Washington recommend waiting another month after the epidemiological turning point before beginning to lift restrictions. In Russia’s case, this would be early July. The logic here is that the number of active cases will approach zero after some amount of time (24 days for Moscow and 30 days for the country as a whole). It’s then advisable to wait another two weeks while the last patients are still contagious (and then an additional 14 days, in case they manage to infect anyone who goes undiagnosed). Once these conditions are met, it can be assumed that the domestic spread of the disease has ended, making it possible to lift restrictions and prepare instead to catch isolated cases brought in from abroad.
An epidemic that hasn’t been fully suppressed threatens new hidden but powerful outbreaks. It will be difficult to battle new waves of the disease: an estimated half of all transmitted infections comes from asymptomatic patients (spread almost immediately after they unknowingly contract the disease). In the event of a large-scale outbreak, doctors and state officials will not have enough resources to identify everyone who’s come into contact with the infected. If infection chains cannot be disrupted, the epidemic will spread uncontrolled once again, necessitating another round of quarantines.
Are the Russian authorities considering all these nuances?
Apparently not. Russia’s criteria for easing coronavirus restrictions do not include the number of locally active cases. German officials, on the other hand, have made the number of active cases central to decision making about lifting containment measures.
Russia’s methodology relies on another vital indicator of the coronavirus: the actual or “effective” transmission rate, known as Rt (not to be confused with “R0,” pronounced R-naught, which is the basic reproductive number, referring to how many people one carrier will infect). Unfortunately, federal regulators in Russia have proposed a dangerously simplified means of calculating this coefficient: dividing the number of recorded cases in a region in the past four days by the number of cases recorded in the four days prior.
This methodology does not take into account:
- Delays in collected data. Recorded cases capture only some of the actual infections that occurred 10–22 days earlier. We don’t exactly know how the virus is spreading now (in regions that are already easing containment measures, new waves could already be underway).
- Underestimations of the real number of infections (patients with weak symptoms or no symptoms at all). The Russian authorities plan to compensate for inevitably underestimated cases by increasing the volume of testing (regions wishing to ease containment measures are supposed to be conducting 70–110 daily tests for every 100,000 residents), but higher volumes of testing don’t eliminate the difficulty of randomizing those tests, which can detect outbreaks at an earlier stage.
- Regional officials’ motivations. Local governments in Russia are currently incentivized to underestimate the number of infected people in their regions and conceal the true spread of COVID-19. New models in the U.S., Asia, and Europe for verifying infection data incorporate not just cases, but test-positive rates, hospitalization information, deaths, excess deaths, and other known COVID-19 data that are highly unreliable at Russian medical facilities, making it impossible to use the available information as a sound basis for policy making.
Text by Dmitry Kuznets
Summary by Kevin Rothrock
(1) Active infections
Confirmed coronavirus patients who have yet to recover or die. The figure can be calculated by subtracting the number of recoveries and deaths from the sum of all infections.